Key Takeaways
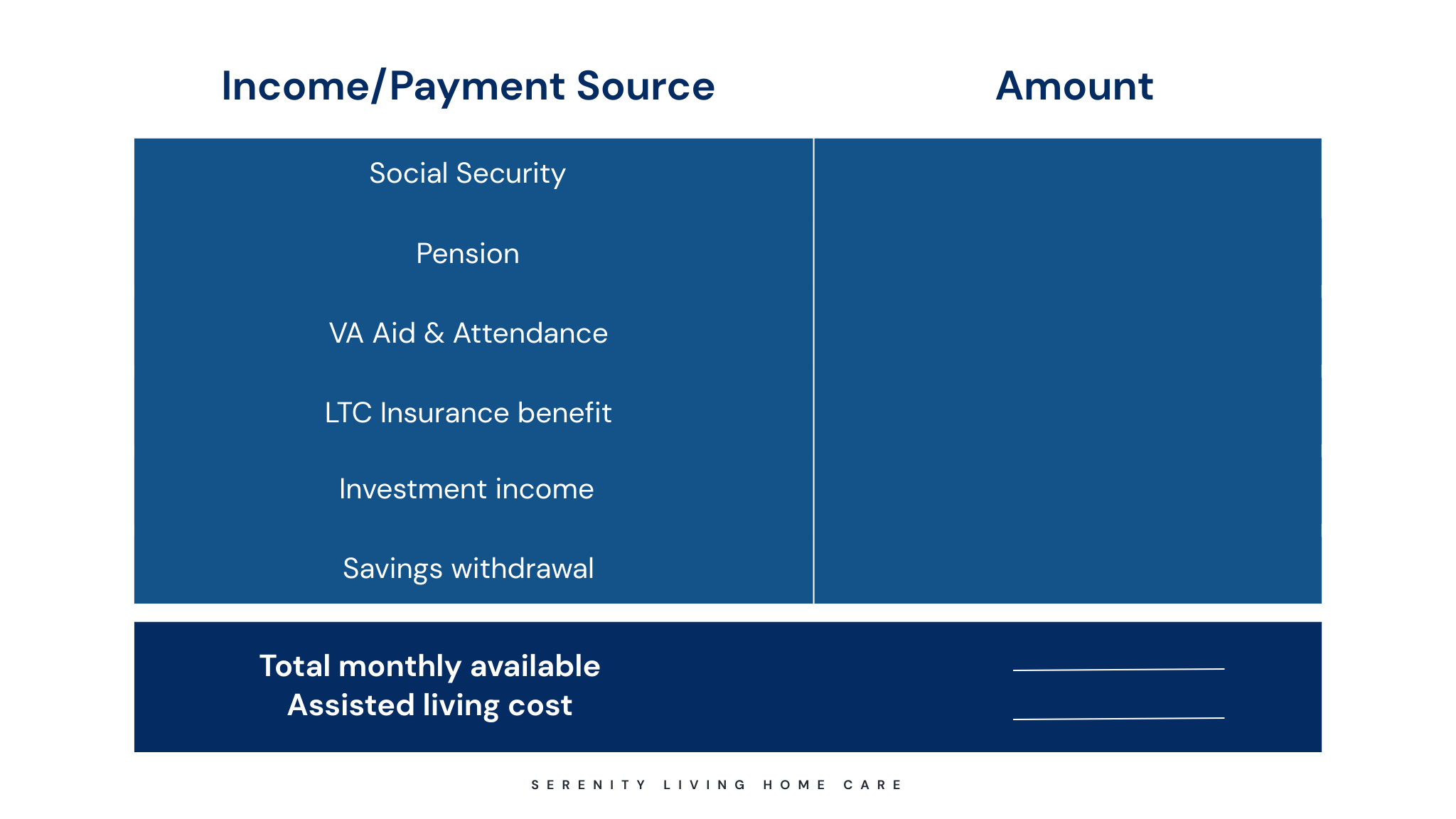
- Families combine savings, insurance, retirement income, and public programs as ways to pay for assisted living costs.
- Medicare doesn’t cover assisted living. Medicaid does if you qualify.
- Plan early to reduce stress and access better care options.
- Most payment strategies involve layering multiple funding sources together.